The State of California declared a state of emergency on Wednesday, after an elderly man, aged 71, who was previously exposed while on a cruise from San Francisco to Mexico in February died from Covid-19 registering the first death in the State of California. He was a resident of Placer County and had underlying health conditions.
In Washington State the number of infected rose close to 80%, to 70 from 39 on Wednesday, March 4, with reports of ten deaths. Six of those fatalities were linked to Life Care Center, a Skilled Nursing and Rehabilitation Center. Washington state declared an emergency late Wednesday.
As reports of the number of cases infected increases, setting fears and anxiety in the hearts and minds of people nationwide is innate. As of this writing Friday, March 6, US reports a total of 14 deaths from the coronavirus. Alex Azar, Health and Human Services Secretary announced the government will ship test kits for 76,000 people to be tested by the end of this week. The US Senate unanimously approved $8.3 billion in emergency spending for the coronavirus outbreak and was approved by President Donald Trump.
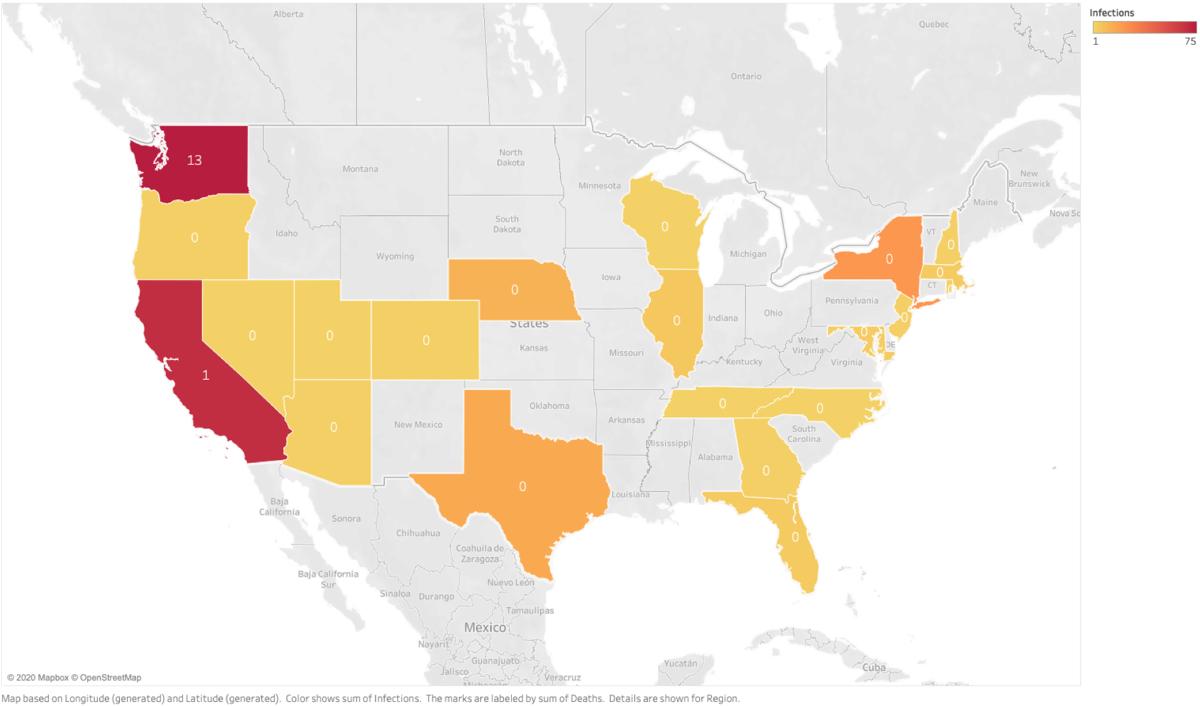
This is what the outbreak spread look like for the rest of the country
Assisted Living and Retirement Communities are inadvertently positioned to become epicenters of coronavirus outbreak. It is estimated that more than 2 Million people live in more than 28,000 residential care facilities in the United States. According to National Center for Assisted Living, the average typical resident is an octogenarian and female.
Already severely constrained with limited resources, a crisis like this is bound to put an immense degree of unplanned and unexpected demands on the workforce. Of utmost importance is the safety and well-being of their elderly residents and caregivers. But battling the outbreak crisis, and continuing perform routine activities, while maintaining a sense of calm and control is a herculean task.
Providers are ordaining the necessary operational changes, taking appropriate precautionary and preventive steps to keep their workforce and elderly residents safe, while devising strategies to keep their organizations braced for a potential outbreak scenario.
What are elderly care providers proactively doing to stay prepared?
1. Continuously Monitoring for Updates and Advice from CDC, City and County Health Departments
Most facilities recognize the need for up-to-date information and advisory on the state of coronavirus and more specifically for the spread-rate and patterns. Having current and accurate information from the right sources is extremely critical in these times. There is a lot of information on the web today making families and residents anxious. Providers are also weighed down by “fear” that is being caused by rumors and misinformation. This further adds to the challenge of filtering out noise from much needed facts and managing communication and expectations of the families and the elderly residents.
Most facility owners, administrators and leadership teams are solely relying on the directives and information from CDC and State and County Health Departments which tends to be more reliable.
Reports of Recovery are important too…
While reports of virus migration and infections are important, of equal importance are reports of recovery amongst infected patients. The good news is with the timely and drastic measures taken by the Chinese government, the outbreak is showing signs of containment in China, indicating that at some point further down the line, there will be a trend reversal in other parts of the world. However, in the short term, prevention is the perhaps the best and only way to contain the migration.
So far, at least 15 people with confirmed coronavirus infections in the United States are said to be showing signs of recovery. Six people in California, four people in Nebraska, two people in Illinois, one each in the states of Arizona, Wisconsin and Washington are recovering.
According to the report from Chinese center for Disease Control and Prevention, which studied 44,672 cases, the elderly, aged 65 and above are more than 10 times likely to be susceptible to the coronavirus compared to younger people.
The US has so far reported about 230 cases of infections and 14 deaths. Based on the known data so far approximately 50% of these fatalities is now considered amongst the elderly. That is a fatality rate of about 6%. However, given how early it is in the process, and as more tests are conducted, the fatality rate is expected to go down significantly. A Medium post by Dr. David Katz, Director, Yale Prevention Research Center, debates on the point of risk distortion and presents an interesting contrast to other epidemics.
Another important point of contention is the stoking of panic that is creating a stigma within our societies. Isolation and retraction from a stigma can be more precarious if people hesitate to come forward and report on their illness. The World Economic Forum released a guideline that articulates the “Dos” and “Don’ts” of which can be found here.
Stories of massive sell-outs of disinfecting wipes, hand sanitizers and over the counter medications are further adding to the frenzy and not helping the situation either. Communities after communities are stockpiling essential supplies like water, toilet paper and food. It is important to watch for CDC Alert levels as a reliable indicator of the level of crisis.
Careful planning and NOT desperation is needed at this hour and people have to be mindful of that.
2. Educating Caregivers
Caregiver safety and well-being is now, more than ever, the top concern for all facility owners and administrators in the face of this crisis. On the frontlines, they are at elevated risk of exposure for themselves and their families — many of who have younger children. All providers are taking extra steps on educating their caregivers and staff on the coronavirus. “We are sending text messages to all caregivers and giving instructions on how best to avoid the virus for them and our clients”, said Craig Falk, CEO and Owner of Craig Cares, a Home Care Agency based in Roseville, CA.
Allaying caregiver fears and helping them brace for their daily activities are a crucial part of this education. The three things caregivers are being advised to do frequently is a) Wash hands with soap for 20 seconds b) Use Hand Sanitizer c) Avoid touching face, eyes or noses.
Monte Coffman, Executive Director of Windsor Place Companies, based in Coffeyville, KS, said “We are increasing managerial observations. We are making sure adequate supplies of universal precaution equipment are made available to staff. We are also equipping all staff with the latest instructional information from CDC.”
3. Review and Reassessment of Policies and Procedures
On this front, the good news is, many elderly care facilities are prepared. Most providers have well defined protocols, policies and procedures to handle epidemics. They are introducing additional processes to keep the caregivers regularly informed and updated. “We have not formally reviewed our care plans as we already have all the necessary protocols in place. Although if we find this virus is different in any way we may reconsider”, says Adam Waskow, Owner and Administrator of Three Homes Village in San Rafael, CA
Some facilities have created task force teams. The main purpose of these task force teams is processing and parsing the streams of information coming from a variety of local, regional and now global sources and to devise strategies and action plans to mitigate potential risks. “We have a task force team, that includes our leadership, infection prevention specialists and medical directors” — adds Monte Coffman.
4. Monitoring Business Impact
While a large majority of the providers are not experiencing immediate short-term impact to their businesses, they are concerned about a potential increase in the operational costs and increased demands on an already thinly stretched workforce. “It is not clear what role insurance will play in this situation and we are waiting for further guidelines and instructions from authorities. Thankfully, we have no reported cases of coronavirus within our community and we have been continuously assessing the threat. But we could be contemplating caregivers performing their daily routine activities in hazmat suits should the situation change, which can be a huge change”, said Jeffrey Dillon, Executive Director of Portola Gardens, an Assisted Living Facility based in South San Francisco.
Many facilities are reducing or limiting facility tours in order to limit the exposure both to their residents and the visitors. Home care agencies are projecting that more seniors may prefer to receive care in their homes. This can further intensify the demand for caregivers in the market where they already in severe short supply.
5. Using Technology
Technology is playing a critical role, especially for timely communications, whether it is from authorities or for downstream communications with clients, families and caregivers. Hospitals and Doctors are encouraging patients to consult over phone first, before making a trip to the hospital or clinic.
Kaiser Permanente, the largest managed care organization based in 8 states, including California, Washington, Oregon and Texas, is offering and relying on telehealth for patients showing symptoms and are quarantined in their homes. Many hospitals and medical centers are offering services over phone, video, chat and chatbots.
Passive monitoring technology products can be a huge help with elderly clients and residents. “Applications like Zemplee can help seniors remain at home where they are safe from infection”, notes Craig Falk.
As new reports of Covid-19 infections and fatalities come in and the risks to the elderly population continues to grow, the spotlight focuses on elderly care providers. The most recent update on the Life Care Center, sheds light on some of the challenges elderly care providers are facing and their readiness to counter and combat major epidemics.
Families are anguished ~ rightfully so. Reassurance and confidence that elderly care providers can deal with an outbreak with competency and completeness is expected and understandable.
Facilities on their part need to assuage families’ concerns. Communication can play a huge role. But but most definitely, caregiver education and timely dissemination of information, an encore review of policies and procedures, and reassessing emergency preparedness is not a bad idea.
Staying calm, prepared an in control is the need of the hour.

